Ten years ago, East Texans lucky enough to survive a cerebral aneurysm had to travel to Dallas or to a few selected medical centers in the nation for the delicate surgery. But now Tyler has six neurosurgeons and one interventional neuroradiologist performing these medical interventions almost daily.
People suffering a cerebral aneurysm – a weakening in a blood vessel in the brain – have a high death rate. However, education, awareness and improved medical procedures have slowly increased odds for survival.
Dr. Thomas W. Grahm, a neurosurgeon with East Texas Medical Center Neurosurgical Institute for eight years, performs about 30 aneurysm surgeries in Tyler each year.
“The main thing about an aneurysm is that it is a treatable disease and our outcomes are at least comparable, and often better, than other comparable centers for this kind of surgery,” the Wichita Falls native said following surgery on an East Texas man.
“We compare favorably even with large academic centers because we have the resources necessary to take care of these complex patients.”
Grahm, a graduate of Fort Worth’s O.D. Wyatt High School, the University of Texas at Arlington and University of Texas Medical School in Galveston, praised the resources available in Tyler.
“We have a neuro ICU, specialized nursing staff, specialized equipment and a specialist (Dr. Kurt Reuland with Tyler Radiology Associates) for interventional neuroradiology,” he said.
“Our outcomes are certainly better than those for centers which do not have such specialized resources,” Grahm said.
With the addition of Reuland’s specialty, he said, the volume of aneurysm procedures will increase in Tyler hospitals.
Grahm trained under Dr. Robert Spetzler at Barrow Neurosurgical Institute in Phoenix, Ariz. Spetzler was the subject of a book titled ” The Healing Blade” by Edward J. Sylvester.
“The residency program at Barrow Neurosurgical Institute is the most difficult program to get into, and this speaks well for the person who is accepted,” Spetzler said.
“We are very proud of Tom’s performance during residency, as well as his accomplishments as a clinical neurosurgeon.”
Married and the father of three boys, Grahm explained how aneurysms are rated. He said the Hunt and Hess Scale for Subarachnoid Hemorrhage (bleeding in the brain) has been the model since the 1960s. The grading goes from Grade 0 with no bleeding to Grade 5 which is a deep coma.
He said his success rate for aneurysm patients never bleeding (Grade 0) is 90-plus percent, while a Grade 1 (a rupture with moderate headache) is about 85 percent. For a Grade 2 (moderate to severe headache and rupture) the success rate is 70-75 percent; and for a Grade 3 (severe headache, lethargy or confusion) it is 50-60 percent. For a Grade 4 (comatose) and Grade 5 (deep coma), it decreases to 20 percent or less.
Grahm said these survival rates are on the same levels with some of the top centers in the United States.
The Handbook of Neurosurgery by Dr. Mark S. Greenberg, M.D., reports patients admitted to a hospital with Grade 1 or 2 aneurysms have a death rate estimated at 20 percent, but this decreases to 14 percent with an operation. The devastating effects of an aneurysm are shown in a book titled “Neurology for the Non-Neurologist ” which reads “…the mortality rate at eight months was approximately 50 percent , with one-quarter of the patients being able to return to work and one-quarter of being significantly disabled. The outcomes appear to be improved by the effective surgical clipping of the aneurysm.”
Grahm said an aneurysm can happen at any age, but rarely in children. He said aneurysms are most prevalent in those around 60 years of age.
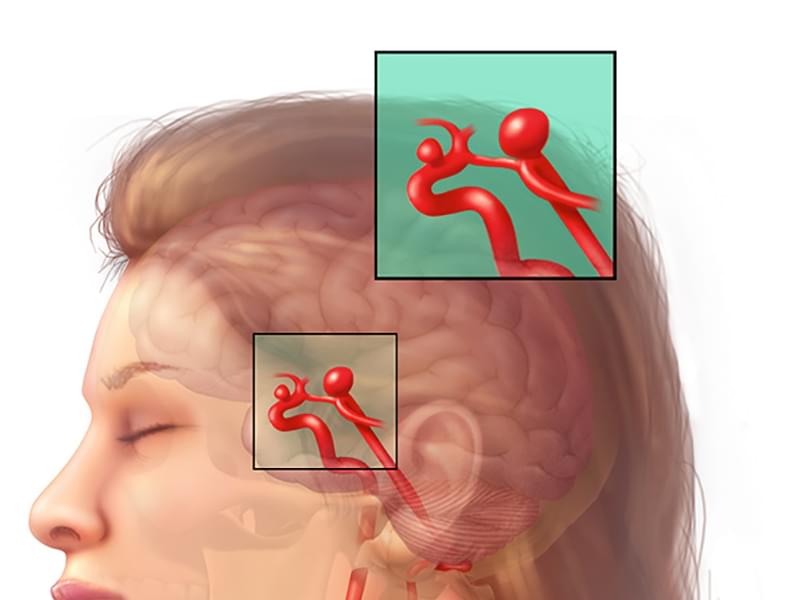
He said aneurysms form from a defect in the artery wall. The artery itself is made of three layers. The intima is the innermost lining. The muscle is the next layer, and the external hard covering is the tough part of the artery.
“Aneurysms are caused by a defect in the muscle layer which basically splits apart and then the thin inside part of the vessel balloons out,” he said.
Grahm said, “The longer we live the more likely we are to get a defect in the artery wall and the more likely we are to get an aneurysm. ” He said conditions like high blood pressure, smoking, wear and tear, and genetics contribute to causing aneurysms.
“We still have a high instance of death with aneurysm, with an estimated 40-50 percent of people dying when they have hemorrhaging from an aneurysm,” he said. “They never make it to the hospital, they just die where they are. That number has always been true and is probably true today. No matter what you do it can happen so quickly and unless you are standing in the emergency room, there is no way to take interventions to stop death in these cases.”
Grahm said what has really improved is those getting to the hospital, receiving treatment and then surgery. “The good news is that a lot more people are getting to the hospital. People are better educated about the classic symptoms for an aneurysm today than they were 20 years ago. When a patient says, “I have just had the worst headache of my life…it’s like a bomb went off in my head,” they should seek immediate medical help,” he said.
“Making an early diagnosis and administering early treatment helps with the survival rate,” he added. ” Also, the more people who survive an aneurysm and talk to friends about their medical problems, the more people are aware that sudden onset of severe headaches could be an aneurysm.”
The only cure for aneurysms has been surgery but during the past 10 years interventional neuroradiology using platinum coils is an alternative course helping improved survival rates in some cases.
Aneurysm surgery generally takes about three hours, with the surgeon using a microscope to see the tiny blood vessels. First step in the surgery is to cut back the scalp; then the skull is opened with a surgical saw.
Tiny titanium clips with jaws are used to obliterate the aneurysm with microinstruments. The aneurysm looks like a balloon with a skinny neck and that area is where the clips are used.
“The ideal is to put the clip across the neck of the aneurysm to shut off the blood supply before the aneurysm breaks, which would cause hemorrhaging,” he added.
“In brain surgery, the brain is unforgiving. With aneurysm surgery – and if you lose one small tiny 1 millimeter area of an artery during aneurysm clipping which sometimes is totally unavoidable – the patient can end up with a stroke (lack of oxygen to the brain) and they can end up in a permanent coma. It’s disheartening and luckily doesn’t happen often, but it does happen.”