A neurosurgeon from Barrow Neurological Institute stressed the importance about stroke warnings along with focusing on a national drive called “Stroke Attack.”
Joseph M. Zabramski, M.D., chief of neurovascular surgery at Barrow, told the Tyler Morning Telegraph during an interview the American Heart Association recommends:”we start calling strokes ‘stroke attacks’ to get the public aware of the urgency to get to a hospital. They want the public to understand that stroke attacks need immediate medical treatment just as heart attacks. The sooner you get to the hospital, the better.”
Dr. Zabramski later spoke to medical personnel at East Texas Medical Center’s Pavilion Conference Center on “Spontaneous Intracranial Hemorrhage: Etiology and Management.” The subject matter covered the study, cause and management of strokes.
During the interview he said warning signs include sudden headaches, sudden loss of function on one side of the body, including motor or sensor functions, sudden inability to speak or any sudden change in level of consciousness. He also said strokes are more age-related. “The older a person is, the more likely they are going to suffer a brain hemorrhage. Under the age of 30 it is about 2 per 100,000 individuals, but at ge 80 and over it is 250 per 100,000.”
Zambramski said, “Spontaneous intracerebral hematoma accounts for only about 10 percent of al strokes but is associated with disproportionately high rates of poor outcomes. Mortality approaches 50 percent at 30 days with only 10-20 percent of surviving patients having a good outcome.”
He said recent studies have drwan attention to the fact that more than one-third of the patients who die or have poor outcomes are admitted soon after a hemorrhage in relatively good condition – alert with or without mild confusion. “The management of this group of patients and the role of surgery in their treatment urgently needs further study,” he added.
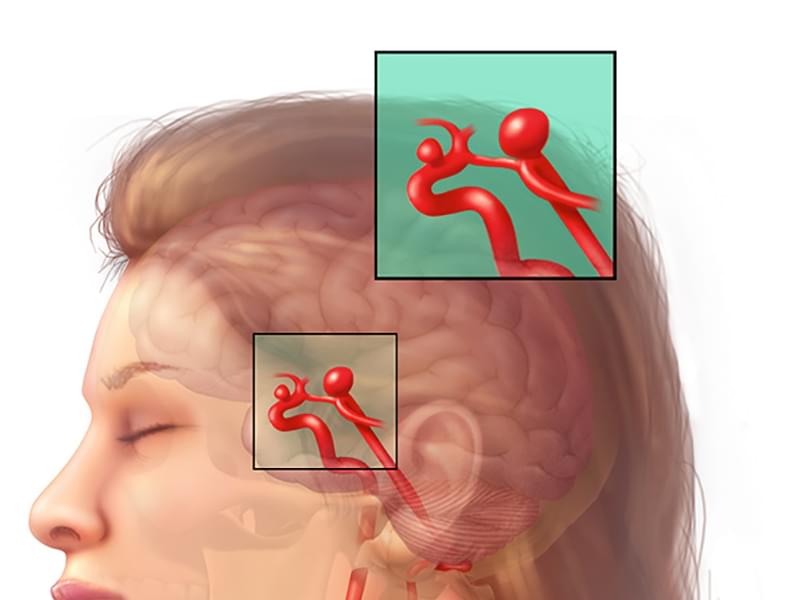
Zabramski, a member of the American Stroke Council and on the editorial board of the journal Stroke said strokes are the third leading cause of death and disability in the United States. About 20-30 percent of strokes are due to a hemorrhage in the brain, “:and those are called hemorrhagic strokes. We have made a lot of progess in the treatment of ischemic strokes (lack of blood flow), but we made very little progress of the treatment of these hemorrhagic strokes.”
“We have good treatments now for strokes that result from blockage of a blood vessel, but we are investigating how to improve the outcomes of the patients with the hemorrhagic type, where the blood vessel actually ruptures and causes bleeding into the brain.”
“We realized in these studies a lot of patients came in looking very, very good and later on deteriorated. So there must be some better treatments we can offer. And as a result of that experience, the American Heart Association has developed a stroke council. One of the first tasks the stroke council was given was to come up with a series of recommendations on how to treat theses hemorrhagic strokes – spontaneous intracranial hemorrhages,” he said.
Zabramski said, “We began to realize how little information there was on the best ways to treat these strokes, so we are doing some preliminary studies right now, gathering data that we can go to the National Institute of Health to ask for funding to examine whether surgery might benefit these patients or new drugs might benefit these patients, or whether the use of a catheter to pull the blood out of the brain and reduce the mass effect created by the hemorrhage might improve outcome.”
“The outcome for these patients is very poor. I think it is initially less than 50 percent of the folks have a good outcome.”
“What we are discovering is that if patients are completely awake and alert when they come in and have a small hematoma (less than 20 centimeters in volume, a little less than an ounce), those patients almost all have good outcomes. If patients come in with a very severe depressed level of consciousness, that is what we call a deep coma, there is no hope,” he said.
“So now we can concentrate on the group in between to see if treatment can imrpove their outcomes.”